🧾 Quick Summary
Diabetes increases your risk of gum disease, dry mouth, infections, and tooth loss
Oral symptoms may be early signs of uncontrolled blood sugar
Regular dental care and blood sugar management help protect your mouth
If you have diabetes, your oral health might be at greater risk than you realize. This guide breaks down how diabetes affects your teeth and gums, the signs to watch for, and how to protect your smile.
Here’s a little known fact few dentists like to share: even when you stay on top of your oral health care at home, you can still have oral health issues. That’s because other factors might be contributing to the problem.
One of the most researched systemic conditions for connections with gum disease is diabetes mellitus. Per the Mayo clinic, people who have diabetes frequently have gum disease, too. The connection could be how diabetes reduces the body’s ability to fight off infection, which leads to gum infections.[i]
What is Diabetes and What Are The Different Types?
Key Things to Know:
Diabetes mellitus is a systemic condition that causes high blood sugar and is categorized into four types: prediabetes, type 1, type 2, and gestational diabetes.
Type 2 diabetes is the most common, often linked to obesity and lifestyle factors, while prediabetes indicates elevated blood sugar not yet at diabetic levels.
Gum disease (periodontal disease) includes gingivitis and periodontitis, and diabetes is a contributing factor to its development and progression.
Let’s take a closer look at diabetes mellitus. Diabetes mellitus, or diabetes, is a systemic disorder that causes elevated levels of glucose in the body. It is classified into four types.[ii]
- Prediabetes: A diagnostic blood test called hemoglobin A1c (HbA1c) measures the amount of blood sugar attached to hemoglobin. [iii] A normal range is between 4% and 5.6%. Prediabetes is someone who has a higher HbA1c than normal but is not high enough to be classified as diabetes and treated with medication (5.7%-6.5%).
- Type 1: Previously known as juvenile diabetes, as it develops early in life, this type is an insulin-dependent form of diabetes due to the pancreas' inability to produce insulin for the body.
- Type 2: This is the most common type, with approximately 90-95% of diabetics being classified as type 2 according to the Center for Disease Control (CDC).[iv] The body can initially produce insulin, but the cells do not respond to insulin as needed, creating insulin resistance. This type generally develops slowly and later in life and is typically in relation to obesity and lack of physical activity.
- Gestational: This type develops during pregnancy. Individuals with gestational diabetes are at a greater risk of developing type 2 diabetes.
What is Gum Disease?
Periodontal disease refers to two specific conditions: Gingivitis and periodontitis. Gingivitis is classified by red, swollen, or bleeding gums and is reversible with appropriate home care. Periodontitis is a more serious condition, typified by bone loss and gum recession which can lead to tooth loss. Periodontitis is chronic and should be treated at regular intervals by your dental team.[v]

How Is Gum Disease Linked to Diabetes?
Key Things to Know:
Diabetes and gum disease worsen each other and need constant care and monitoring.
Diabetes damages oral health, causing swollen gums, slow healing, dry mouth, and tooth decay.
Uncontrolled diabetes triggers chronic inflammation, leading to bleeding gums, loose teeth, and bad breath.
It’s helpful to understand that the relationship between diabetes and periodontitis and even gingivitis and diabetes is considered a bidirectional one.[vi] This is to say that people diagnosed with both diabetes and periodontal disease have two chronic conditions, each of which may affect the other. Both require frequent professional evaluations, in-depth patient education, and consistent educational reinforcement by healthcare providers.[vii]
In addition to the impacts on your overall health, there’s a range of oral complications from diabetes that affect the gums, teeth, and surrounding tissues, including:
- Puffiness or swollen gums
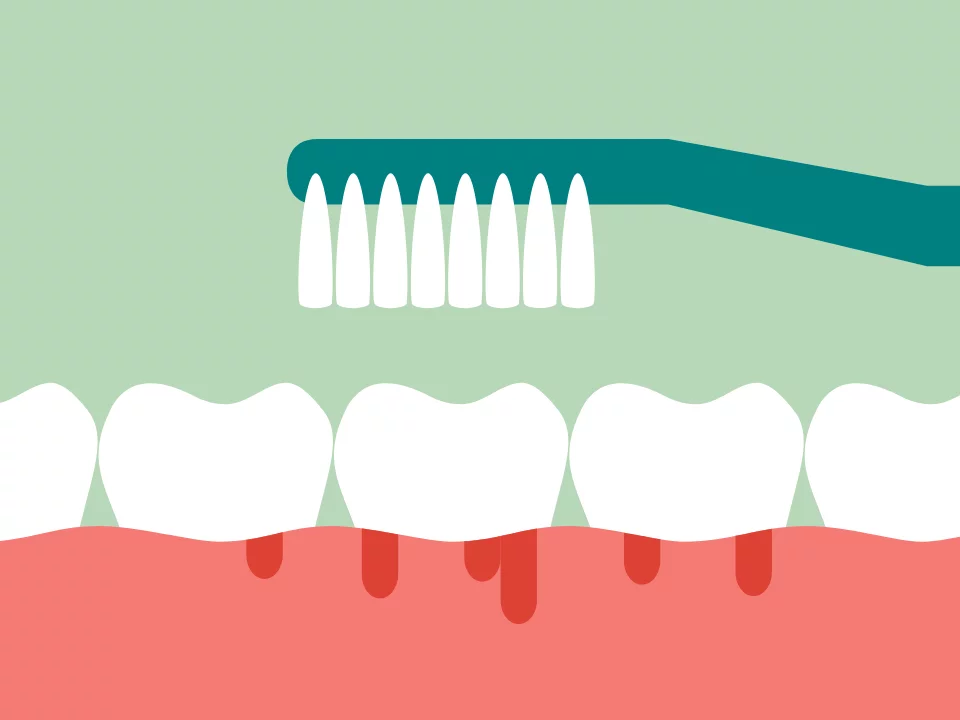
- Bleeding gums
- Burning sensation in the mouth
- Reoccurrence of mouth sores
- Reduced salivary gland function
- Altered taste
Many times, the inflammation in some patients’ mouths has a direct connection to their type 2 diabetes. Exacerbation of periodontal disease is considered a complication of diabetes when other factors such as poor home care or genetics are not the likely cause. Also, research shows that patients with poorly controlled type 2 diabetes are at greater risk for periodontal disease progression than patients with well-controlled type 2 diabetes.[viii]
Does Diabetes Affect Your Gums?
Also, gums and diabetes have a relationship, too. Complications from diabetes do not help the body heal the inflammation in gums. Diabetic patients often have a wound healing impairment, so they recover slower from mouth ulcers and gum trauma than people who don’t have diabetes. The infected gum tissue then traps excess bacteria in the gum pockets, which is the area of the gums next to the tooth. The more bacteria present in the gum pockets, the worse the inflammation of the gums from periodontal disease gets. Left untreated, patients could have receding gums from diabetes.
However, that’s not the only way the Mouth-Body Connection between gum disease and diabetes impacts oral and overall health. Both diabetes and periodontitis can stimulate the chronic release of proinflammatory cytokines, which have a harmful effect on gum tissues. [ix] Some patients in this situation may experience bleeding gums as one of their diabetes symptoms when brushing or flossing, as well as permanent teeth that feel loose, and gum recession.
Does Diabetes Cause Bad Breath?
Another oral manifestation of diabetes your dental team might notice is bad breath. Bad breath and diabetes are common companions, particularly breath that smells fruity or acetone-like.[x] This nail-polish essence on the breath could indicate a dangerous level of ketones, putting the body at risk for diabetic ketoacidosis (DKA).
Does Diabetes Cause Dry Mouth?
Also, xerostomia, or dry mouth, another side effect of diabetes, can cause bad breath. Saliva helps control the bacteria growth in your mouth. When salivary production is lowered, it allows the bacteria to grow, which contributes to an unpleasant odor, known as halitosis. In addition, dry mouth increases the risk of tooth decay for patients with diabetes. Furthermore, diabetics are already at a higher risk for dental decay due to high levels of glucose in their blood. When combined with dry mouth, the risk tooth decay with diabetes only grows higher. [xi]
Does Diabetes Cause Tooth Loss?
Can Gum Disease Cause Diabetes?
Key Things to Know:
Gum disease can worsen blood sugar control, making diabetes harder to manage.
Plaque and bacteria from gum disease can trigger inflammation that affects the whole body, including diabetes risk.
Research links severe gum disease to higher HbA1c levels, raising the risk for type 2 diabetes and diabetes complications.
It is clear that diabetes causes teeth and gum problems, but what about the other way around? Can gum disease cause diabetes? What about gum disease and prediabetes? As we mentioned before, gum disease and diabetes is bidirectional, meaning they travel on a two-way street. So, while there is no causal link established by research, gum disease also affects type 2 diabetes. That’s because your body is a system, meaning that what affects one area of the body will have effects on the other areas.
How Does a Dentist Help with Diabetes?
Dentists have a significant role in diabetes management stemming from their treatment of your gum disease. [xvii] The treatment of periodontitis includes oral hygiene instructions by your dental hygienist or dentist, a nutrition assessment and accompanying information on the role of your diet, and a periodontal cleaning of the teeth and gingival tissues. At each cleaning, the pocket depth of your gums should be assessed via probe readings, and the teeth will be cleaned by an ultrasonic device and hand instrumentation. An antibacterial mouth rinse such as chlorhexidine gluconate may be prescribed to control specific bacteria found in periodontal disease.
In addition to the cleanings, other treatments might be recommended for your gum disease treatment. Surgical or non-surgical intervention may be prescribed. Non-surgical therapy includes scaling and root planing, localized antibiotics, and gum irrigation. Research supports that active therapy such as scaling and root planing significantly reduces HbA1c levels at three months, with even more reduction after six months.[xviii]
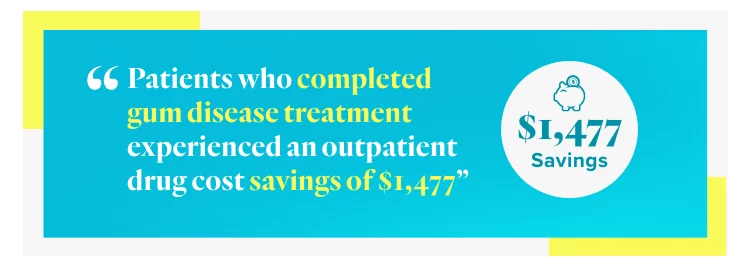
In addition to the health benefits, the dentists’ role in diabetes management has other benefits, too:
Lower annual medical costs: Diabetic patients who completed periodontal treatment saved $2,840, or 40 percent, compared to those who did not complete treatment (per United Concordia Dental, a dental wellness company in Pennsylvania).
Reduced outpatient drug costs: Patients who completed gum disease treatment also saved $1,477 in outpatient drug expenses.
It is interesting to note the following:
Study size: Over 91,000 members had both type 2 diabetes and periodontal disease.
Treatment completion: Only 913 patients completed gum disease treatment.
Lack of treatment: Over 90,000 diabetics did not complete gum disease treatment.
Key insight: Avoiding periodontal treatment offers few patient benefits.
Main takeaway: Treating gum disease has major health and financial benefits, potentially improving outcomes for people with systemic conditions like diabetes.
What Will Your Dentist Want to Know?
Can You Treat Gum Disease & Diabetes at Home?
Key Things to Know:
Good oral hygiene (brushing, flossing, regular dental visits) reduces mouth inflammation and helps manage diabetic symptoms.
Frequent brushing (three times a day) lowers diabetes risk, while poor oral care and missing teeth increase it.
Other tips: Replace toothbrushes regularly, use fluoride mouthwash, eat a nutrient-rich diet, and quit smoking to protect oral and overall health
Getting your oral health back in tip-top shape is an excellent way to protect your teeth and gums. It also will decrease inflammation in your mouth. That effort includes a reinvigorated devotion to consistent and comprehensive home care and seeing your dentist regularly.
Speaking with Your Dentist About Gum Disease and Diabetes
Now that you have a better understanding of the link between diabetes and your oral health, feel free to ask your Smile Generation-trusted dental team about your oral and systemic health. You should probably ask if you are at risk for gum disease and if that means you might be at higher risk for diabetes and other systemic conditions. If you recognize any of the oral symptoms described, ask your dentist or hygienist about them, so they can examine the situation and determine if there is a problem.
Should you need periodontal disease treatment, you can find a dentist near you with comprehensive treatment plans, smoking cessation plans, affordable financing options, and more. You can also use our Find a Dentist tool to find a trusted dentist in your area.
Find your trusted, local dentist today!
Sources
- [i] Mayo Clinic. (2021). Oral health: A window to your overall health. MayoClinic.org. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475. Accessed April 28, 2025.
- [ii] Darby, M. L., Walsh, M. M., Bowen, D. M., & Pieren, J. A. (2020). Dental hygiene: Theory and practice (5th ed.). Elsevier/Saunders.
- [iii] Darby, M. L., Walsh, M. M., Bowen, D. M., & Pieren, J. A. (2020). Dental hygiene: Theory and practice (5th ed.). Elsevier/Saunders.
- [iv] Mealey, B. L. (2006). Periodontal disease and diabetes. Journal of the American Dental Association, 137(10), 26S–31S. https://doi.org/10.14219/jada.archive.2006.0404. Accessed April 28, 2025.
- [v] United Concordia Dental. (2014). The mouth: The missing piece to overall wellness and lower medical costs. Accessed April 28, 2025.
- [vi] Mealey, B. L. (2006). Periodontal disease and diabetes. Journal of the American Dental Association, 137(10), 26S–31S. https://doi.org/10.14219/jada.archive.2006.0404. Accessed April 28, 2025.
- [vii] Mealey, B. L. (2006). Periodontal disease and diabetes. Journal of the American Dental Association, 137(10), 26S–31S. https://doi.org/10.14219/jada.archive.2006.0404. Accessed April 28, 2025.
- [viii] Hallmon, W. W., & Mealey, B. L. (1992). Implications of diabetes mellitus and periodontal disease. The Diabetes Educator, 18(4), 310–315. https://doi.org/10.1177/014572179201800409. Accessed April 28, 2025
- [ix] Hallmon, W. W., & Mealey, B. L. (1992). Implications of diabetes mellitus and periodontal disease. The Diabetes Educator, 18(4), 310–315. https://doi.org/10.1177/014572179201800409. Accessed April 28, 2025.
- [x] Darby, M. L., Walsh, M. M., Bowen, D. M., & Pieren, J. A. (2020). Dental hygiene: Theory and practice (5th ed.). Elsevier/Saunders.
- [xi] Darby, M. L., Walsh, M. M., Bowen, D. M., & Pieren, J. A. (2020). Dental hygiene: Theory and practice (5th ed.). Elsevier/Saunders.
- [xii] United Concordia Dental. (2014). The mouth: The missing piece to overall wellness and lower medical costs. https://www.unitedconcordia.com/docs/united%20concordia%20oral%20health%20whitepaper.pdf. Accessed April 28, 2025.
- [xiii] Mayo Clinic. (2021). Oral health: A window to your overall health. MayoClinic.org. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475. Accessed April 28, 2025.
- [xiv] Hall, K., & Sinha, S. (2018). What you need to know about gum disease. Everyday Health. https://www.everydayhealth.com/gingivitis/what-you-need-know-about-gum-disease/. Accessed April 28, 2025.
- [xv] Dansinger, M. L. (2020). The hemoglobin A1c test & chart. WebMD. https://www.webmd.com/diabetes/glycated-hemoglobin-test-hba1c. Accessed April 28, 2025.
- [xvi] National Institute of Diabetes and Digestive and Kidney Diseases. (June 2016). Diabetes statistics. U.S. Department of Health and Human Services.
- [xvii] Mayo Clinic. (2021). Oral health: A window to your overall health. MayoClinic.org. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475. Accessed April 28, 2025.
- [xviii] Darby, M. L., Walsh, M. M., Bowen, D. M., & Pieren, J. A. (2020). Dental hygiene: Theory and practice (5th ed.). Elsevier/Saunders.
- [xix] United Concordia Dental. (2014). The mouth: The missing piece to overall wellness and lower medical costs. https://www.unitedconcordia.com/docs/united%20concordia%20oral%20health%20whitepaper.pdf. Accessed April 28, 2025.
- [xx] United Concordia Dental. (2014). The mouth: The missing piece to overall wellness and lower medical costs. https://www.unitedconcordia.com/docs/united%20concordia%20oral%20health%20whitepaper.pdf. Accessed April 28, 2025.
- [xxi] American Diabetes Association. (2024). Statistics about diabetes. https://diabetes.org/about-diabetes/statistics/about-diabetes. Accessed April 28, 2025.
- [xxii] Chang, Y., Lee, J. S., Lee, K. J., et al. (2020). Improved oral hygiene is associated with decreased risk of new-onset diabetes: A nationwide population-based cohort study. Diabetologia, 63, 924–933. https://doi.org/10.1007/s00125-020-05112-9. Accessed April 28, 2025.
Smile Generation blog articles are reviewed by a licensed dental professional before publishing. However, we present this information for educational purposes only with the intent to promote readers’ understanding of oral health and oral healthcare treatment options and technology. We do not intend for our blog content to substitute for professional dental care and clinical advice, diagnosis, or treatment planning provided by a licensed dental professional. Smile Generation always recommends seeking the advice of a dentist, physician, or other licensed healthcare professional for a dental or medical condition or treatment.





.png)