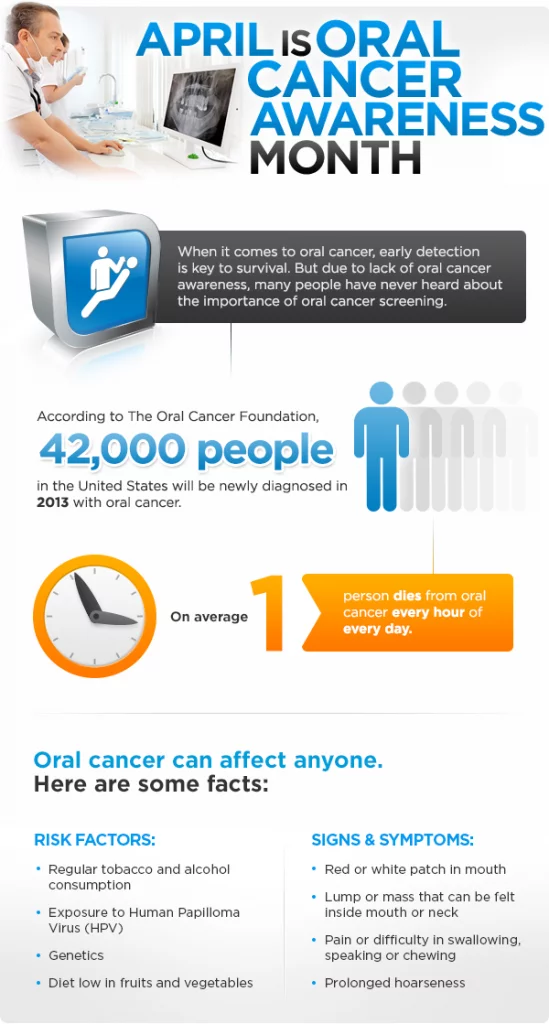
April is oral cancer awareness month. Cancer is a life-threatening illness that affects any part of the body. Protect yourself by learning all you can about oral cancer and by having regular dental exams.
Cancer: Know All You Can About It
Cancer is one of the scariest words in our language. If you’re one of a growing number of people determined to take an active role in your health care now and in the future, you’ll want to learn what you can about one of the principal killers in developed nations today. Knowledge is power; let’s arm ourselves with as much knowledge as we can. We will begin with an overview and then apply the information to a more specific type: oral cancer.
Cancers are a class of diseases characterized by the uncontrolled division of cells and the ability of these cancerous cells to spread. They can grow into nearby tissue through a process known as invasion, or they can be transported through the bloodstream or lymphatic system (a complex system of glands and ducts active in the body’s defense against disease) to distant areas by what is called metastasis. I’ll attempt to provide what we know today about this major threat.
There are many types of cancers; how severe the symptoms are generally depends on the nature of the malignancy, which refers to cancerous cells that usually have the ability to spread, invade, and destroy tissue. Most cancers can be treated, and some even cured, depending on the type, location in the body, and at what stage the cancer is diagnosed. However, once diagnosed, cancer is usually treated with a combination of surgery, “chemotherapy” (drugs that destroy cancerous cells), and “radiotherapy” (killing cancerous cells with radiation).
How is a Normal Cell Transformed?
The unregulated growth of cells that characterizes cancer is caused by damage to DNA — the stuff that genes are made of. The genes are the command machinery that informs the cells what to do. Mutations to the DNA alter and damage proper cell function. Many mutation events may take place to transform a normal cell into a malignant one. What causes these mutations to occur? They can be caused by radiation, chemicals, or physical agents known as carcinogens or by certain viruses that are able to insert their own genetic material into human cells. There are two alarming characteristics of mutations:
- They can occur spontaneously
- They may be passed down from one cell generation to the next
Cancer: A “Multifactorial” Disease
There are many reasons or factors that cause normal cells to mutate into cancerous ones. Among the most important are:
- Predisposing Factors — an innate capacity to develop disease that can be triggered under certain conditions, e.g., genetics (genes that are altered or mutate tend to occur along family lines), and
- Risk Factors — conditions or behaviors that increase the possibility of disease, e.g., smoking, chewing tobacco and alcohol use, diets low in fruits and vegetables, viral infections — primarily the human papillomavirus “HPV 16” (the same one that’s been in the news lately which causes cervical cancer in women), and an immune (protective) system that is not functioning normally in response to infections or inherited disease.
Oral Cancer & Precancerous Conditions
Now that we have more of a background about cancer, its causes, and its risk factors, let’s take that knowledge and apply it to a specific area, the mouth.
Oral cancer accounts for roughly 3% of all cancers in men and 2% in women. Men still outnumber women two to one, but this is changing as women become more exposed to the same risk factors as men. Like all cancers, oral cancer is associated with aging. Did you know that more than 90% of all oral cancers occur in individuals over 40? We now know that African Americans have a higher incidence than Caucasians, and a disturbing number of cases in young people, regardless of ethnicity, have been seen in recent years.
Get familiar with the main areas where oral carcinomas (cancers) occur:
- Oral cavity proper (the mouth),
- Lip and tongue
- Pharynx (back of the mouth and throat).
You might say that the mouth and lips are accessible for direct examination all the time by routine visits to the dentist. Thinking along those lines, it’s probably easy for a dentist to notice anything unusual in the mouth within a matter of months. Here’s the scary aspect of oral cancer: it is not usually detected until a late stage. So despite all the advances in treatment, survival is poor, with only 58% surviving five years after treatment.
Most oral cancers are “squamous” (small scale-shaped) cell carcinomas, occurring in the lining of the mouth and are often preceded by identifiable surface changes (lesions) of the oral membranes. White or red patches begin to form in the pre-cancerous stage, and as the cancer develops, a non-healing ulcer may appear.
Research has shown us that men are twice as likely to develop oral cancer as women, and men over the age of 50 are the most at risk. Tobacco (including smokeless tobacco) and excessive alcohol consumption are the strongest risk factors. In recent years, human papillomavirus (HPV) has been found to cause an increasing number of cancers of the oropharynx. It is related to the rise in throat cancers in nonsmoking individuals who drink moderately. However, only a small percentage of HPV infections develop into cancer.
The tongue, particularly the sides, is the most common site for oral cancer, with the floor of the mouth (under the tongue) coming in second. Lip cancers primarily affect the lower lip, and frequently there is a history of chronic sun exposure and preceding damage, which shows up as scaling and crusting at the site. The thing to remember here is that recurring ulcers in the lip area can also be mistaken for cold sores. Since the tongue has a rich blood supply and lymphatic drainage (the lymphatic system is a major component of our immune protection system), 30% of cancers have spread or metastasized by the time they are diagnosed. That’s a frightening fact. Now let’s take that fact a step further — up to 15% of people diagnosed with oral cancer are typically found to have a second primary cancer.
However, when detected early while a lesion is small, the survival rate exceeds 80%. So bear in mind that early detection is key. If you notice any unusual lesions (sores or ulcers) or color changes (white or red patches) anywhere in your mouth that do not heal within two to three weeks, get to your dentist or physician as soon as possible.
Diagnosis Can Be Complicated
Earlier, we explained that oral cancers are most often detected when they are at a late stage, with early diagnosis only taking place in about one-third of the cases. Unfortunately, recognition is complicated. Why? Because the early signs can mimic harmless sores that occur in the mouth, such as canker sores, minor infections, or irritations from biting or even certain foods. When we’re given a proper oral cancer exam which includes the oropharynx, the health care professional will feel the neck for lumps; inspect the lips and all inside surfaces of the mouth, including the tonsils at the back of the throat.
Further, we must remember that oral cancers can occur on any surface that lines the mouth and throat, with the tongue being the most common site. These changes can appear as white or red patches, ulcers, and lumps that may or may not be associated with discomfort or pain.
An appropriately trained dentist will know how to diagnose oral cancer and evaluate any such changes that persist for more than two to three weeks. A definitive diagnosis requires the microscopic examination of a piece of the lesion (tissue biopsy). This is a procedure usually carried out with local anesthesia, numbing the involved site with the removal of a sample or all of the abnormal tissue if small enough. The tissue specimen is then sent to the lab for analysis, where it undergoes microscopic evaluation for a more thorough diagnosis.
Treatment of Pre-Cancerous Conditions
Pre-cancerous lesions must be assessed by biopsy (tissue sampling for disease). There is no need for biopsy if pre-cancerous changes disappear by removing irritants, e.g., tobacco, alcohol, biting, or other chemical or physical irritants. Follow-up is necessary to determine a frequency for continued monitoring and evaluation. This will, of course, depend upon the findings at the time of biopsy. The ultimate treatment of pre-cancerous lesions is surgical removal; however, the use of lasers has been very helpful. Diets, vitamins, and other drug or chemical approaches have not been useful.
If there is a reason to delay biopsy, other techniques are available to help evaluate a suspicious lesion. While these non-invasive “adjunctive” techniques help shed light on a suspicious lesion, they do not substitute for biopsy confirmation. These FDA-approved devices include the use of light reflections, tissue staining (tolonium chloride), cytology (brush biopsy), and fluorescence. These adjunctive techniques do not require anesthesia and help accelerate the need for further testing or referral. These techniques are available to general dental practitioners; however, biopsy remains the gold standard.
Once the diagnosis is definitive, the extent of the disease has to be determined so that a treatment plan and prognosis can be formed. Staging is the term used to describe the level a cancer has reached. Involved in staging are clinical, microscopic findings, and imaging with techniques such as magnetic resonance imaging (MRI). Depending upon the stage, your health care professional will formulate a treatment plan that will most likely include considerations for surgery and/or radiation and/or chemotherapy. With all treatments, the teeth and membranes of the mouth must be protected from further incidence of decay, gum disease and other infections, dryness of the mouth, and other more subtle changes.
A treatment team usually comprises surgeons, radiation and medical oncologists (cancer specialists), dentists, dental hygienists, nurses, and other professional specialists.
What to Expect During an Oral Cancer Screening
Your dentist will inspect your face, neck, lips, and mouth to look for any signs of oral cancer. First, they will feel the external area under your jaw and the outside of your neck with both hands, checking for lumps (enlarged lymph nodes) that may suggest inflammation. Oral cancer may be suspected if these nodes are painless but hard and enlarged. You will also be asked to stick out your tongue so it can be checked for swelling or abnormal color or texture. Then, using a small piece of gauze, your dentist will lightly pull your tongue to each side to fully visualize its edges, a common location for precancerous and cancerous lesions to occur. Additionally, your dentist will visually examine the roof and floor of your mouth, the back of your throat, the tonsils, and the gums for any discolorations or lesions.
Early Detection with VELscope Oral Screening
Smile Generation-Trusted Dentist Dr. Ashley Elizondo, owner of Pearland Dentists and Pearland Modern Dentistry & Orthodontics in Pearland, TX, shared how she and her team successfully utilize VELscope screenings as an adjunct to the traditional head and neck exam. "It is our standard of care as a diagnostic tool. We screen all new patients and we screen returning patients at least once a year. For patients who are high risk, such as tobacco users, we recommend screenings every six months. A few years ago, I had a patient who had a lesion I could see during the traditional head and neck exam, but after using the VELscope, I learned she had two lesions. The patient was referred to a specialist; the lesions were both due to HPV and fortunately were not malignant. This was an "ah-ha" moment for us. Over the years, we've referred multiple patients for further evaluation. The pictures we take with VELscope allow for better communication with our specialist and provides us with an added advantage to better assess our patients before referring. It is such a valuable screening tool because it allows us to see things not visible during a traditional head and neck exam which allows us to provide a more comprehensive exam and help create happier, healthier patients.”
VELscope VX is a wireless handheld device that uses tissue fluorescence to identify oral abnormalities early. Many times, VELscope VX can detect abnormalities months or even years before they can be identified with the naked eye! VELscope VX is painless and quick; it can be used in only two minutes! While it does not diagnose oral cancer, it can help detect precancerous and cancerous lesions that we may not be able to see otherwise. If you are a high-risk patient for oral cancer (alcohol or tobacco user, or high risk for HPV), it is recommended you have the VELscope VX exam done with your oral cancer examination. Remember, early detection yields the best results!
Alcohol consumption increases the risk factor for cancer of the oral cavity, pharynx, and larynx. The liver and the mouth break down alcohol into a substance known as acetaldehyde. Acetaldehyde is toxic to the human body. It causes cancer by damaging the body’s DNA and preventing cells from preparing the damage. Alcohol also inhibits the body from breaking down nutrients associated with the risk for cancer.
But it is possible that resveratrol — an antioxidant found in grapes used to make red wine — can make tumor cells more sensitive to chemotherapy. Resveratrol is a natural antibiotic. It helps prevent damaged cells in plants from replicating. The thought is it can help fight cancer by suppressing the growth of cells. It might also as well as diminish cancer from invading healthy cells.
Consult your dentist to discuss your questions about oral cancer and oral cancer month. Or, check out The Smile Generation to find a dentist near you for all your oral cancer and April cancer awareness month questions and concerns. You can read patient reviews, peruse staff bios, and schedule an appointment online with a click of your mouse.
Find your trusted, local dentist today!
Smile Generation blog articles are reviewed by a licensed dental professional before publishing. However, we present this information for educational purposes only with the intent to promote readers’ understanding of oral health and oral healthcare treatment options and technology. We do not intend for our blog content to substitute for professional dental care and clinical advice, diagnosis, or treatment planning provided by a licensed dental professional. Smile Generation always recommends seeking the advice of a dentist, physician, or other licensed healthcare professional for a dental or medical condition or treatment.